Abstract

Introduction: Venous thromboembolism (VTE), defined as pulmonary embolism (PE) and lower extremity deep vein thrombosis (LE-DVT), is a potentially preventable complication for cancer patients undergoing systemic therapy. The Khorana score (KS) is the most used risk assessment model (RAM) to predict venous thromboembolism (VTE) in ambulatory cancer patients. Potential limitations of the score include modest discrimination and small proportion of people developing VTE in the high-risk subgroup. We aimed to derive and externally validate a more precise yet equally RAM for VTE through two unique healthcare systems.
Methods: We derived a parsimonious RAM using the cancer registry-linked electronic health records from the Harris Health System (HHS, N=9,916) and validated it using the Veterans Affairs national healthcare system (VA, N=78,892) from 2011-2020. Patients were included if they had their first-ever newly diagnosed cancer and received first-line systemic therapy within 1 year of diagnosis. Index date was the time systemic therapy and all covariates were extracted on or prior to index date. Incident VTE and PE/LE-DVT were defined using our computable phenotype algorithm (PMID: 35647478). When tested against the gold standard of chart abstractor review in a random sampling of 400 patients at each site, the algorithm had a positive predictive value (PPV) of 98% and sensitivity (Sn) of 96% at HHS; and a PPV of 90% and weighted Sn of 82% at VA.
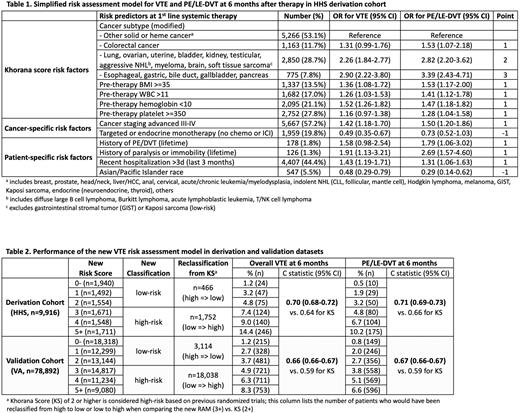
For RAM derivation, 34 candidate predictors of VTE were initially chosen by clinicians and 11 final covariates were selected by the LASSO regression via cross-validated optimal lambda.1se. The original KS components were forced into the final model. For external validation, bootstrapped time-dependent c statistics and calibration curves for 6-month VTE and PE/LE-DVT risk were used to assess model discrimination and fit. Dichotomized risk strata using integer scores were created and compared against the KS. Complete data analysis was performed without imputation.
Results: The median follow-up for continuous VTE assessment were 11.5 months (IQR 5.7-21.1) for HHS and 14.9 months (IQR 5.9-31.9) for VA. At 6 months, there were 656 (6.6%) VTE (including 448 (4.5%) PE/LE-DVT) and 1,094 (11.0%) deaths in HHS, and 3,209 (4.1%) VTE (including 2,474 (3.1%) PE/LE-DVT) and 13,792 (17.5%) deaths in VA. Due to differences in healthcare systems, the two cohorts had very different baseline characteristics in demographic, cancer, systemic therapy, and co-morbidity. Patients from HHS were younger (median age 55 vs. 67), more diverse by sex (female 56.6% vs. 4.9%) and race/ethnicity (15% vs. 71% White, 52% vs. 5% Hispanic, 27% vs. 5% Black, 6% vs. 2% Asian/Pacific Islander [API]), compared to the VA.
When assessed at the time of systemic therapy initiation, the new RAM in derivation cohort included components of the KS with modified cancer subtype, cancer staging, systemic therapy class, history of VTE, history of paralysis/immobility, recent hospitalization, and API race (Table 1). Due to lower incidence of VTE in VA, re-calibration-in-the-large (intercept only) optimized the overall fit of the model in external validation. The c statistic for the VTE outcome was 0.70 in HHS and 0.66 in VA (compared to 0.64 and 0.59, respectively, for KS). Furthermore, the new RAM appropriately reclassified 27% of patients from the previous risk groups and increased the proportion of VTEs in the high-risk group from 36.7% to 68.0% in the validation dataset (Table 2).
Conclusions: Using easily extractable data from two independent healthcare systems, we successfully derived and externally validated a RAM for VTE in a diverse population by sex and race with all cancer types (including hematologic malignancy) and receiving all types of modern systemic therapies (including immune checkpoint inhibitor, targeted therapy, endocrine therapy) in addition to chemotherapy. It stratified approximately 50% of patients with all cancer types receiving all types of modern systemic therapy into a high-risk group with a 6-month VTE risk of 7-11%, and the other half into a low-risk group with a corresponding risk of 3%. The RAM had improved performance over the original KS and doubled the number of VTE events in the high-risk stratum. The incorporation of this modified RAM can lead to improved risk stratification and personalized decision-making for pharmacologic thromboprophylaxis.
Disclosures
Carrier:BMS: Consultancy, Honoraria, Research Funding; Servier: Consultancy, Honoraria; Sanofi: Consultancy; Pfizer: Consultancy, Honoraria, Research Funding; Bayer: Consultancy, Honoraria; Leo Pharma: Consultancy, Honoraria, Research Funding. Flowers:Denovo Biopharma: Consultancy; TG Therapeutics: Research Funding; Sanofi: Research Funding; Pharmacyclics: Research Funding; Kite: Research Funding; Janssen Pharmaceutical: Research Funding; EMD: Research Funding; Xencor: Research Funding; Ziopharm: Research Funding; Burroughs Wellcome Fund: Research Funding; 4D: Research Funding; NPower: Current holder of stock options in a privately-held company; Acerta: Research Funding; Adaptimmune: Research Funding; Spectrum: Consultancy; SeaGen: Consultancy; Pharmacyclics/Janssen: Consultancy; Iovance: Research Funding; Guardant: Research Funding; Morphosys: Research Funding; Gilead: Consultancy, Research Funding; Karyopharm: Consultancy; Foresight Diagnostics: Consultancy, Current holder of stock options in a privately-held company; Takeda: Research Funding; Eastern Cooperative Oncology Group: Research Funding; Cellectis: Research Funding; Amgen: Research Funding; Genmab: Consultancy; Pfizer: Research Funding; Genentech/Roche: Consultancy, Research Funding; Celgene: Consultancy, Research Funding; Allogene: Research Funding; National Cancer Institute: Research Funding; V Foundation, Cancer Prevention and Research Institute of Texas: CPRIT Scholar in Cancer Research: Research Funding; BeiGene: Consultancy; Abbvie: Consultancy, Research Funding; Bayer: Consultancy, Research Funding.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal